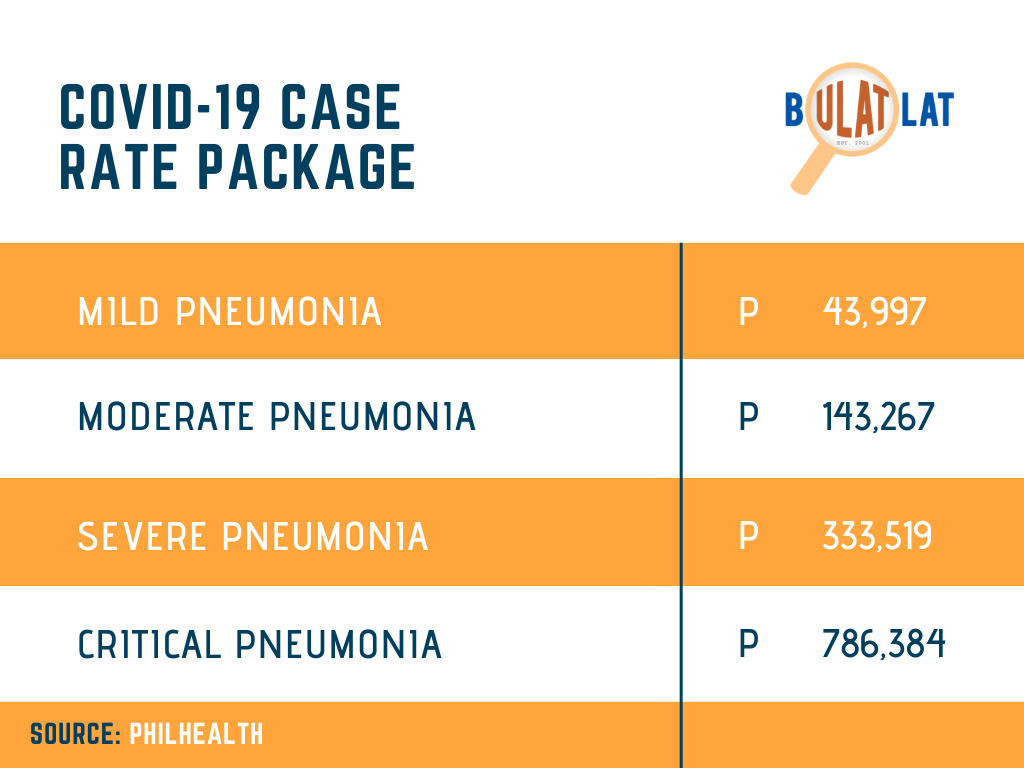
This means that only those with mild pneumonia could be fully covered by PhilHealth. Those with moderate, severe and critical pneumonia will have to shell out payments from their own pockets, ranging from 35 percent to 88 percent for an eight-day confinement. For severe and critical pneumonia, Philhealth will only cover nine percent to 21 percent of the total cost for a 16-day hospitalization.
By JANESS ANN J. ELLAO
Bulatlat.com
MANILA – With the new “package” for COVID-19 patients offered by the Philippine government’s health insurance system, groups have expressed concerns on its impact on poor communities and low-income families as the country continues to grapple with the spread of the pandemic.
In a statement, ACT Teachers Rep. France Castro said families who barely have enough to buy food and even middle-income earning families cannot afford to shoulder the costs of hospitalization and treatment that COVID-19 entails as hospital bills can reportedly go as much as P3.8 million.
“With that cost, there would be people who would be more afraid of the cost for its testing and treatment of COVID-19 than being infected by the virus,” said Castro.
Per its Advisory No. 2020-022, PhilHealth said it will shoulder the full cost of treatment of all COVID-19 patients due to the “novelty and the wide range of severity of the disease,” for which they have no existing case rate or package. Medical expenses of both public and private health workers, meanwhile, will still be shouldered even after April 14.
Philhealth will offer the new case rates for COVID-19 patients who will be admitted to hospital care starting April 15, an official explained in a DZBB interview.
Last month, PhilHealth announced that it will release P30 billion to hospitals in its fight against the deadly virus. On Monday, the government health insurance system said it has released over P8 billion out of the P30 billion budget. But the per-case rate must be pursued to provide “some sustainability” to the anti-COVID-19 campaign as they do not know “how long this pandemic is going to last,” said its president Ricardo Morales.
Under this scheme, reimbursements are provided through predetermined fixed rates for specific diseases.
The packages for COVID-19 treatment, however, are a far cry to the reported costs of hospitalization.
News reports say that COVID-19 hospitalization can go from P93,000 for an eight-day confinement to as much as P3.8 million for a 16-day stay at the hospital.
This means that only those with mild pneumonia could be fully covered by Philhealth. Those with moderate, severe and critical pneumonia will have to shell out payments from their own pockets, ranging from 35 percent to 88 percent for an eight-day confinement. For severe and critical pneumonia, Philhealth will only cover nine percent to 21 percent of the total cost for a 16-day hospitalization.
“How does government expect to stop the further spread of the virus if the people are more afraid of the medical cost for testing and treatment of COVID-19 than the virus itself?” said Castro, adding that without mass testing, proper quarantine, and medical support to the people, she said that affected families will be buried in huge debt and the government will not likely “succeed in defeating this virus.”
Case rates means higher out-of-pocket spending
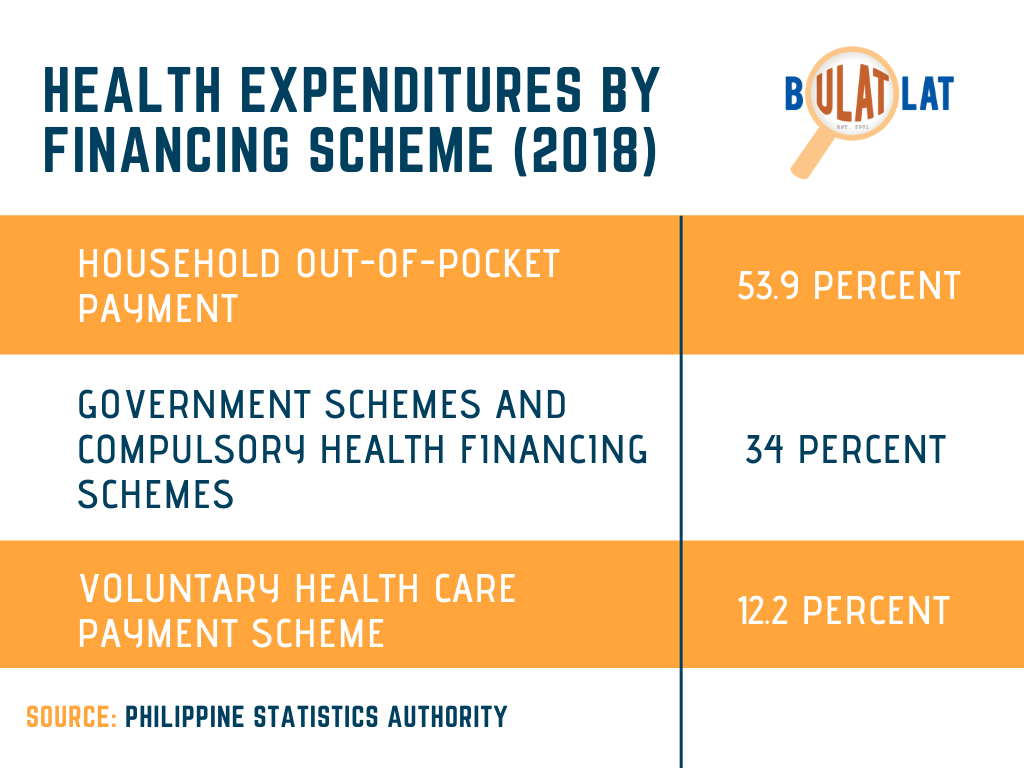
Since 2011, when PhilHealth’s health financing shifted to “case rate,” health advocacy groups pointed out that the scheme resulted in increased out-of-pocket expenses for patients.
PhilHealth first introduced case rates that will aim to provide “optimal financial protection” through consistent and fixed rates of benefits through its Circular No. 21 series of 2011. Two years later, it came up with another circular that is aimed to eventually phase out the fee-for-service mechanism.
Read: Offer free health services, not PhilHealth coverage — health groups
According to the 2018 Philippine Health Systems Review published by the World Health Organization, PhilHealth reimburses 30 percent to 60 percent of the hospital cost, leaving 40 percent to 70 percent for patients to bear.
In 2018, the per capita health spending in the Philippines increased by 8.3 percent. This translates to a total of about P413 billion out-of-pocket expenses that Filipinos spent for health-related concerns or about P7,496 per person.
These out-of-pocket spending were mostly spent on pharmacies and private hospitals.
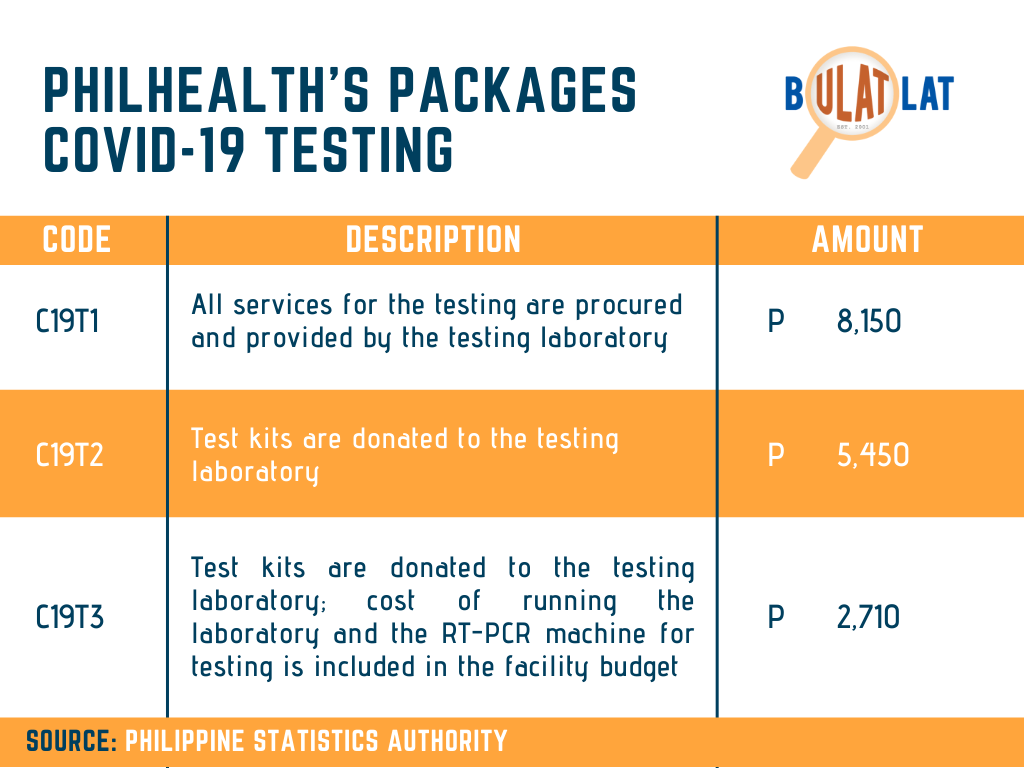
Still, amid a pandemic, the Philippine government, through Philhealth, has shifted its health financing to a per-case scheme. It has issued a list of case rate packages and a separate circular detailing case-based payment for COVID testing.
Not responsive to public health system
Santiago Dasmariñas Jr., secretary general of Courage, a nationwide union of government workers, said the public health system “remains at a pitiful level,” especially with PhilHealth providing limited funding now for COVID-19 patients when the mass testing is set to start this week.
At least 65 percent of confirmed COVID-19 cases were brought to private hospitals, as of March 20, according to independent think-tank Ibon Foundation. This, Ibon said, shows how the government has passed on the “duty of caring for these patients” even as insurance claims are “too low for them.”
“The passing on of big private hospitals to government hospitals shows how profit-oriented the Philippine health care system is and how DOH [Department of Health] willingly bows down to the demands of these big private hospitals,” Ibon Foundation said in its earlier report.
Infographics by Alyssa Mae Clarin
The post Philhealth’s COVID-19 package means more debt for middle-income, poor patients appeared first on AlterMidya.